As urgent care centers face an increasing demand for services, reducing patient wait times has become a top priority. Long wait times not only affect patient satisfaction but also indicates operational inefficiencies and can result in revenue loss. The question that we face next is, what will it take to reduce patient wait times and correspondingly enhance the overall patient experience? Below is the 5S framework strategy that can significantly reduce wait times and improve operational efficiency.
Streamlined Pre-Registration and Online Check-In
Did you know that online check-in can save a patient up to 16 minutes[1] sitting in the waiting room?
With the rise of digital technologies, pre-registration and online check-in systems are revolutionizing the way urgent care centers operate. By enabling patients to complete their details and necessary paperwork remotely, healthcare providers can eliminate front-desk bottlenecks, allowing staff to focus on providing timely care.
Integrating an Electronic Medical Record (EMR) portal into the online system further enhances this process. Patients can update personal information, schedule or change appointments, get e-reports, and even join the queue before arrival. Additionally, automated text reminders keep patients informed about appointment details, reducing confusion and improving overall time management. This seamless digital experience not only minimizes wait times but also empowers patients to manage their appointments with ease.
Virtual Queue Management
Imagine knowing exactly how long your wait will be before you even walk into the clinic. Virtual queue management can make this a reality. Studies show that 83% of patients experience less frustration when they know what to expect regarding wait times.[2]
The adoption of virtual queue management can enable patients to reserve a spot, get information about expected wait time, room availability, and wait remotely, significantly decreasing overcrowding in waiting areas. By integrating this advanced scheduling software, healthcare providers can seamlessly manage patient data, categorize appointments based on urgency, and prioritize critical cases effectively. Dynamic scheduling further enhances this process by allowing real-time adjustments for cancellations and no-shows, ensuring optimal utilization of available time slots. Automated appointment reminders via SMS/email serve as an additional layer of efficiency, reducing no-show rates and maintaining a more predictable schedule. Additionally, incorporating the automated queue management portal with digital display systems on the center can further minimize the need for additional staffing, further streamlining operations.
Streamlined Triage Process
A streamlined triage process is key to reducing wait times and ensuring that patients receive timely and appropriate care. Prioritizing urgent cases right from the start ensures that critical patients aren’t delayed. The implementation of standardized triage protocols guarantees consistency and efficiency in patient assessments, helping reduce variability and avoid delays in treatment.
By leveraging digital tools like online symptom checkers, AI-driven triage systems, and telehealth services, healthcare providers shall accelerate the triage process. AI-based systems can analyze vital signs, medical history, and symptoms to assess acuity levels and predict potential complications, facilitating quicker decision-making. This reduces in-person wait times, ensures rapid assessments, and prevents bottlenecks. Moreover, AI-integrated systems that connect with Electronic Health Records (EHRs) ensure that data is readily available for informed decision-making in real time. This rapid assessment process can quickly categorize patients based on the severity of their conditions. Self-service kiosks can also aid the triage process, allowing patients to check in, report symptoms, and get assessed without further delays at the front desk while allowing medical professionals to focus on delivering care. The combination of AI and digital tools enables urgent care centers to provide timely care and improve patient satisfaction.
Patient Volume Forecasting
Accurate forecasting of patient volumes based on historical data analysis and seasonal & daily variation trends in patient volumes can plays a crucial role in proactive resource planning. A high accuracy level in forecasting can help an Urgent Care Center in preparing for demand fluctuations by allocating adequate staff and medical equipment to cater to the expected volumes. It also helps in allocating appointment slots according to projected demand and capacity constraints. This would have a. direct impact on patient wait times.
Using data to strengthen overall workflow
Data is crucial in identifying inefficiencies and optimizing workflows. By implementing robust data collection and analytics systems, urgent care centers can make strategic decisions that reduce wait times and improve overall operational efficiency. Tracking key process measures such as wait times, treatment durations, and staff utilization as well as tracking flow of patients across work centres/activities can help in uncovering bottlenecks that might be causing delays leading to higher waiting times. It would also help in focusing on improving the bottleneck activities leading to direct reduction in overall cycle time and corresponding wait times.
Conclusion
Are You Ready to Take the Next Step in Reducing Wait Times?
Reducing patient wait times in urgent care centers requires a comprehensive approach—incorporating technology, staff training, and data analytics to optimize patient flow. At Navikenz, we specialize in digital transformation solutions that can revolutionize how healthcare providers operate. From automating patient flow to using AI-powered scheduling and predictive analytics, we offer the expertise necessary to help your urgent care facility achieve seamless operations and deliver an exceptional patient experience.
Are you ready to improve your urgent care center’s efficiency? What will it take to give your patients the best experience, while also optimizing your operations?
Get in touch with us today to explore the future of urgent healthcare management at info@navikenz.com.
References:
[1] https://docresponse.com/blog/how-to-reduce-patient-wait-times/
[2] https://www.unotech.io/5-simple-tips-to-reduce-patient-waiting-time-in-clinics
https://lonestaruc.com/articles/7-best-strategies-to-reduce-care-wait-times/
https://www.wavetec.com/blog/healthcare/improve-patient-flow-in-urgent-care/
https://www.dezyit.com/post/boosting-triage-efficiency-in-healthcare-the-role-of-ai
Urgent care centers operate in a fast-paced, high-demand environment where patient influx can be unpredictable. Managing this demand efficiently requires accurate patient load forecasting. A mismatch between anticipated and actual patient volumes can lead to overcrowding, long wait times, staff burnout, and a decline in patient satisfaction.
The key question for urgent care providers is: How accurate is your patient load forecasting, and how is it impacting your operations?
Is Your Patient Load Forecasting on Track?
Understanding whether your current forecasting methods are effective is crucial. Are you frequently experiencing patient surges that can’t be handled? Do you often have idle staff due to overestimation? Forecasting mismatch can impact both quality of care and financial stability. If your predictions are missing the mark, it’s important to evaluate your forecasting models.
Understanding Typical Patient Load in Urgent Care Centers
In 2022, the UCA Operations Benchmarking Report revealed that the median patient volume for an urgent care center was 56 patients per day[1]. This number can fluctuate based on location, season, and specific healthcare trends. On weekdays, urgent care centers typically see the highest patient load on Monday mornings, with a gradual decrease throughout the week, often experiencing a slight uptick in patient volume on Friday afternoons. During flu season or viral outbreaks, patient volumes can increase by up to 40%[2], overwhelming the system if not properly managed. The demand also tends to peak in the evenings after regular work hours. Understanding these patterns is essential for strategic staffing, inventory planning, and operational efficiency.
Effect on Patient Satisfaction Due to Mismatch in Patient Volume Forecasting
One of the key drivers behind the growing popularity of urgent care centers is their ability to deliver superior patient experience. In an industry often characterized by complex navigation and long wait times, urgent care centers stand out by offering convenience and efficiency. A significant mismatch between anticipated and actual patient volumes can directly impact patient satisfaction in urgent care centers. When patient demand exceeds expectations, understaffing leads to long wait times, rushed consultations, and overwhelmed healthcare providers, resulting in a subpar patient experience. Conversely, overestimating patient volume can lead to inefficient resource utilization, causing unnecessary operational costs without improving service delivery. Patients expect quick and seamless care from urgent care centers, and any disruption whether in the form of extended wait times, lack of available providers, or disorganized workflows can lead to frustration and lower satisfaction scores. Research by American Journal of Managed Care shows that patient satisfaction is highly correlated with wait times and provider engagement[3]; thus, an inaccurate forecasting model can significantly erode trust and loyalty, ultimately affecting repeat visits and word-of-mouth referrals.
Effect of Accurate Patient Load Forecasting
Accurate patient load forecasting is essential for optimizing operations in urgent care centers, directly influencing patient satisfaction, resource allocation, and financial performance. By leveraging historical data, seasonal trends, and AI-driven predictive analytics, UCCs can anticipate patient demand with greater precision. A well-calibrated forecasting model ensures optimal staffing levels, reduces patient wait times, and enhances the overall quality of care. For instance, research indicates that utilizing predictive models can lead to a reduction in emergency department delays by up to 15%.[4] Additionally, a study focusing on urgent care clinics found that machine learning algorithms improved patient volume forecasting accuracy by approximately 23-27% over traditional methods.[5]
Achieving high accuracy in patient load forecasting involves integrating real-time data, considering external factors such as seasonal illnesses or local events, and continuously refining predictive models. Centers adopting advanced forecasting techniques have reported significant improvements in operational efficiency and patient satisfaction. Therefore, embracing sophisticated forecasting methodologies is crucial for urgent care centers aiming for operational excellence and enhanced patient care.
Conclusion: How Is Your Urgent Care Center Performing?
Given the direct impact of forecasting accuracy on wait times, NPS, and overall center performance, it’s crucial to ask:
- Are your patient volume predictions aligning with actual demand?
- How is your forecasting accuracy affecting patient satisfaction and attrition?
At Navikenz, we drive digital transformation to enhance patient load forecasting. Our solutions assist urgent care centers in achieving higher accuracy in demand prediction, enabling better staffing decisions, and improving patient outcomes. If you’re concerned about the accuracy of your patient load forecasting and its impact on your operations, Navikenz can provide an in-depth assessment and tailored solutions to optimize your processes.
Let’s discuss how we can help you improve efficiency and patient care. Contact us at info@navikenz.com.
References:
[1] https://urgentcareassociation.org/wp-content/uploads/2023-Urgent-Care-Industry-White-Paper.pdf
[2] https://www.experityhealth.com/urgent-care-visit-data/
[3] https://www.ajmc.com/view/wait-times-patient-satisfaction-scores-and-the-perception-of-care
[4] https://www.gsb.stanford.edu/insights/predictive-data-can-reduce-emergency-room-wait-times
[5] https://arxiv.org/abs/2205.13067
https://www.immediatecarewestmont.com/what-is-the-busiest-day-of-the-week-for-urgent-care/
In today’s fast-paced healthcare environment, urgent care centers (UCCs) play a pivotal role in providing immediate medical attention for non-life-threatening conditions. However, patient experiences in these settings often fall short of expectations, leading to dissatisfaction and potential disengagement from essential healthcare services. Dissatisfied patients not only deter potential clientele but also adversely affect the Net Promoter Score (NPS), which is a critical indicator of patient satisfaction and loyalty. Therefore, understanding and addressing the primary factors contributing to negative patient experiences is crucial for UCCs aiming to improve care quality and patient retention.
Prolonged Wait Times
A study by the Urgent Care Association found that 64% of the patients rank wait time as the top reason for leaving an urgent care facility without being seen.[1] The wait time is heavily impacted by a mismatch between anticipated and actual patients. When patient demand significantly exceeds expectations, understaffing leads to long wait times, rushed consultations, and overwhelmed healthcare providers, resulting in a subpar patient experience. The lack of a proper appointment and queue management system further deteriorates the situation. Patients today expect speed and efficiency. If their expectations aren’t met, they get disengaged—impacting footfalls and reviews. Negative patient experiences not only increase attrition but also deter potential new patients from choosing your center.
Staff Behaviour
The demeanor and professionalism of healthcare providers directly influence patient satisfaction. Positive interactions, characterized by empathy, respect, and effective communication, can enhance trust and comfort, leading to improved health outcomes. Conversely, negative behaviours, such as rudeness, dismissiveness, or lack of attention, can result in patient dissatisfaction, increased anxiety, and a reluctance to seek future care. Research by the American Journal of Managed Care shows that patient satisfaction is highly correlated with wait times and provider engagement.[2] A survey by the GMR Web Team in January 2021 revealed unpleasant and rude behavior experiences as the key reason for negative patient sentiment.[3]
Environmental Factors
The physical environment of an urgent care center significantly influences patient satisfaction and recovery. Key elements such as cleanliness, noise levels, lighting, and overall ambiance play crucial roles in shaping the patient’s experience. A clean and well-maintained facility not only reduces the risk of infections but also instills confidence in patients regarding the quality of care they will receive. Conversely, inadequate cleanliness can lead to dissatisfaction and a diminished perception of care quality.
Issues in Billing and Insurance Processing
Billing and insurance processing in urgent care centers are often complex and prone to delays, resulting in significant challenges for both providers and patients. Traditional billing processes can lead to inefficiencies, as urgent care centers often rely on manual data entry and paper-based claims, which increase the risk of errors and delays in processing claims. Sometimes claims are denied in the initial stage due to mistakes in coding or billing, and this causes delays in reimbursement and patient frustration. Moreover, navigating the insurance system can be a headache for patients who may face unexpected out-of-pocket expenses due to lack of transparency or insufficient coverage information. In addition, patients also report confusion or dissatisfaction with how their insurance claims were processed, resulting in lower satisfaction levels and increased complaints. These inefficiencies, coupled with the complex nature of the reimbursement system and the need for prior authorization in some cases, can contribute to negative patient experiences, making it essential for urgent care centers to implement better billing practices and more transparent communication regarding insurance coverage to enhance overall patient satisfaction.
Navikenz excels in process re-engineering and IT solutions to address problems impacting patient satisfaction. With our expertise in digital transformation solutions, we help streamline billing processes, reduce patient wait time, and improve forecasting accuracy. Our data-driven solutions enhance operational efficiency, ensuring a smoother patient journey from check-in to reimbursement. By partnering with Navikenz, you can not only address existing inefficiencies but also elevate your center’s overall patient satisfaction, making it a trusted choice for your community.
Contact us today at info@navikenz.com.
References:
[1] https://www.experityhealth.com/blog/solving-the-top-reason-patients-lwbs-wait-time/
[2] https://www.ajmc.com/view/wait-times-patient-satisfaction-scores-and-the-perception-of-care
[3] https://www.gmrwebteam.com/urgent-care-patient-satisfaction-survey-2021#:~:text=Overall%2C%20the%20Net%20Promoter%20Score,was%2077.30%20/100%20in%202020
https://www.hipaajournal.com/effects-of-poor-communication-in-healthcare/
https://www.kff.org/health-costs/issue-brief/americans-challenges-with-health-care-costs/
Urgent care centers play a vital role in providing accessible and efficient healthcare. However, many of them struggle with revenue losses due to write-offs. These write-offs significantly impact financial stability, reducing profitability and hindering growth. To maintain financial health, urgent care providers must understand the primary causes of write-offs and take proactive measures to mitigate them.
What Causes Write-Offs in Urgent Care?
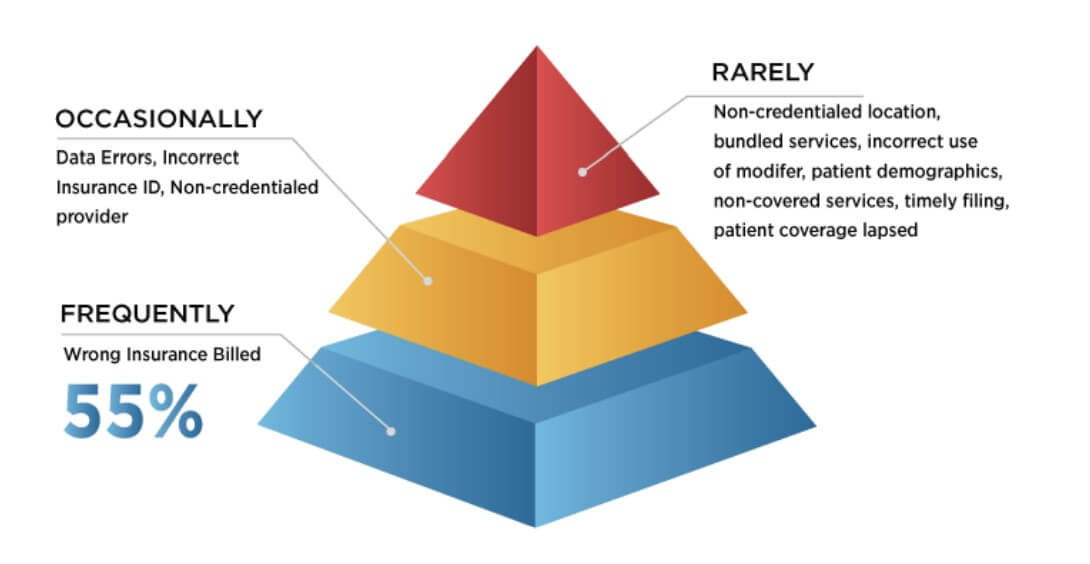
Source: Urgent Care Association) [1]
- Wrong Insurance Billed: One of the primary reasons for write-offs is insurance claim denials. Insurance companies may refuse to pay claims due to incorrect coding, incomplete documentation, or failure to verify a patient’s insurance eligibility. Even minor errors in coding or missing documentation can lead to claim rejections, forcing urgent care centers to absorb the costs. Additionally, if a patient’s insurance coverage is not verified before treatment, the center may unknowingly provide services that are not covered, leading to revenue losses. Another common issue arises when services are billed to the wrong insurance provider, leading to claim denials and revenue loss. Billing errors, including wrong insurance submissions, contribute significantly to financial losses. In 2023, insured patients accounted for 53% of the estimated $17.4 billion in bad debts written off by healthcare providers. [2] As per a survey by the Urgent Care Association (UCA), the most frequent reason cited for these claim denials is the wrong insurance being billed, with nearly half of all respondents indicating this as their most frequent reason.[3]
- Data Errors: These involve inaccuracies in patient or billing information, such as incorrect coding or demographic details, resulting in claim denials or payment delays. A survey from healthcare technology company Solv. found that 44% of patients enter an incorrect address, which leads to a myriad of clerical issues. Another survey by UCA highlighted that data errors and incorrect insurance ID were reported as an occasional problem about 75% of the time.[4]
- Contractual Write-Offs: These occur when there’s a difference between the provider’s charges and the amount agreed upon with insurance companies. For instance, if your center charges $150 for a service, but the insurer’s allowable fee is $100, the remaining $50 becomes a contractual write-off. While standard in the industry, excessive contractual write-offs can indicate unfavorable payer contracts that may need renegotiation.
- Bad Debt Write-Offs (Healthcare Industry-Wide Problem): This category includes amounts deemed uncollectible due to patient non-payment. Factors contributing to bad debt write-offs include economic hardships faced by patients or ineffective collection processes within the center. Notably, hospitals have observed that as patient balances increase, the likelihood of collection decreases Patient statements with balances greater than $7,500 have more than tripled from 5.2% in 2018 to 17.7% in 2021, leading to higher bad debt write-offs [5]. And according to public accounting firm Crowe, self-pay after insurance accounted for nearly 58% of bad debt in 2021 [6], compared with only 11% in 2018. The rise of high-deductible health plans and higher out-of-pocket medical expenses are a few factors driving this trend.
- Timely Filing Write-Offs: Insurance companies impose deadlines for claim submissions. Failing to file within these timeframes results in denied claims, which then must be written off. In general, medicare requires claims to be filed no later than 12 months after the date of service to be paid.
Strategies to Minimize Write-Offs in Urgent Care
Urgent care centers can reduce write-offs by improving documentation accuracy, strengthening insurance verification, and regularly reviewing payer contracts. Effective patient payment plans, proper provider credentialing, and tracking and managing denials help balance revenue and patient acquisition. Leveraging AI-driven billing systems and automated claim tracking can further enhance efficiency. By addressing these factors, urgent care centers can safeguard financial health while continuing to provide quality patient care.
Time to Introspect
- Have you effectively managed to address the issue of write-offs?
- Is the patient management process at your urgent care centers strong enough to take care of insurance mismatches?
- Are your center’s collection efforts effective in reducing write-offs?
Navikenz has designed solutions for Urgent Care Clinics to streamline revenue cycle management, reduce billing errors, and optimize cash flow. To minimize write-offs and unlock sustainable growth, reach out to us at info@navikenz.com
References:
[1] https://urgentcareassociation.org/wp-content/uploads/Finance-v9.pdf
[2] https://www.definitivehc.com/blog/hospital-bad-debt-statistics-you-need-to-know
[3] https://urgentcareassociation.org/wp-content/uploads/Finance-v9.pdf
[4] https://urgentcareassociation.org/wp-content/uploads/Finance-v9.pdf
[5] https://www.healthcarefinancenews.com/news/claims-denials-rise-complicating-revenue-collection-survey
[6] https://www.crowe.com/-/media/crowe/llp/widen-media-files-folder/h/hospital-collection-rates-for-self-pay-patient-accounts-report-chc2305-001a.pdf
The urgent care industry in the United States has experienced remarkable growth over the past decade, nearly doubling from 7,220 centers in 2014 to 15,032 as of January 2025.[1] This rapid expansion underscores the highly competitive and elastic nature of the market, where patient choices are abundant, and switching costs are minimal. In such a dynamic environment, understanding and enhancing patient satisfaction and loyalty are paramount for urgent care centers aiming to differentiate themselves and retain their patient base.
Net Promoter Score (NPS), in particular, is a key metric for urgent care centers (UCCs), providing valuable insights into patient experiences and overall satisfaction. A high NPS indicates positive patient experiences, leading to better retention and strong word-of-mouth referrals. By benchmarking NPS against industry standards, UCCs can identify areas for improvement, set realistic goals, and enhance service delivery. Focusing on NPS helps drive performance improvements and positions urgent care centers as leaders in patient care.
How is NPS Measured?
NPS measures patient loyalty by assessing the likelihood of patients recommending a service to others. Patients are categorized as Promoters (scores 9-10), Passives (scores 7-8), or Detractors (scores 0-6). The NPS is calculated by subtracting the percentage of Detractors from the percentage of Promoters, yielding a score between -100 and +100.[2]
Industry Benchmarks: Where Do Urgent Care Centers Stand?
Analyzing industry benchmarks for Net Promoter Scores (NPS) in urgent care centers reveals a consistent trend of high patient satisfaction and loyalty. According to a 2021 survey by GMR Web Team among 17756 patients, the overall NPS for urgent care centers was 76.5 out of 100, indicating a strong likelihood of patients recommending these services.[3]
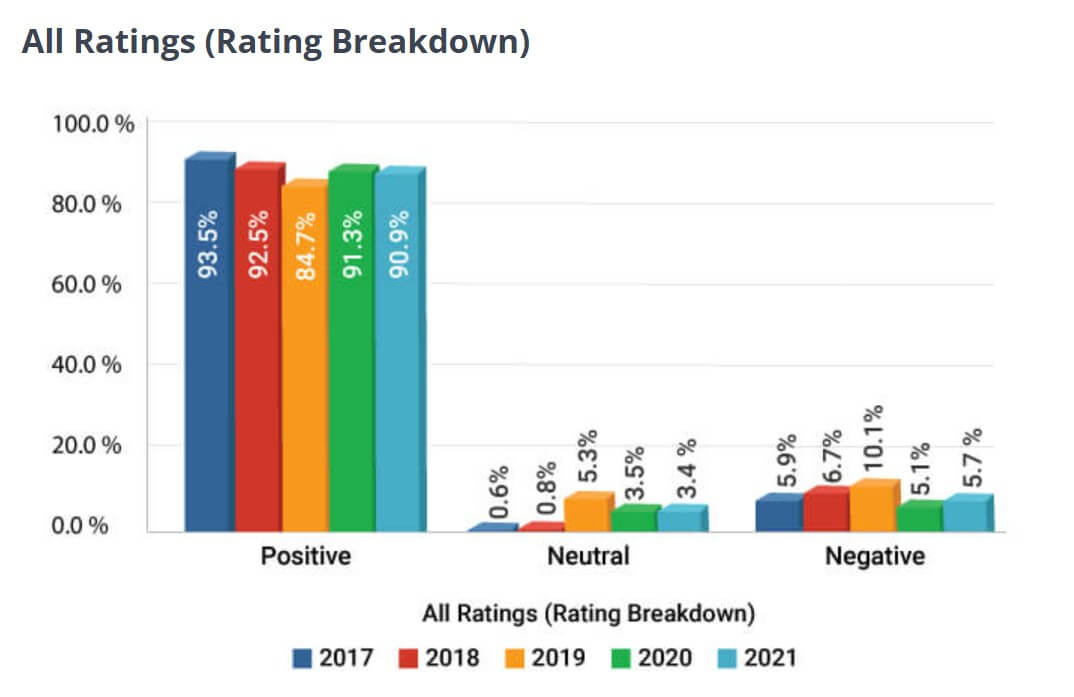
(Source: GMR Web Team)
Similarly, a review of over 928,000 surveys collected through Experity Patient Engagement reported an average NPS of 86 for urgent care centers, further emphasizing the positive patient experiences in this sector.[4] These figures suggest that urgent care centers generally outperform the broader healthcare industry, which has an average NPS of 58.[5]
Maintaining or exceeding these benchmark scores is crucial for urgent care centers aiming to enhance patient satisfaction and foster loyalty.
Improving Your NPS Scores
Enhancing your Net Promoter Score (NPS) is essential for fostering patient loyalty and improving overall service quality in your urgent care center. Implementing strategies such as streamlining patient flow to reduce wait times and problems of over and understaffing, clearly communicating diagnoses and treatment plans, training staff in active listening and empathy, regularly collecting and responding to patient feedback, following up with dissatisfied patients, maintaining a clean and comfortable environment, investing in staff training on patient-centered care and effective communication, and streamlining administrative processes can significantly improve patient experiences. By focusing on these areas, your urgent care center can enhance patient satisfaction, leading to higher NPS, increased patient loyalty, and a stronger reputation in the healthcare community.
Conclusion
It is time to introspect:
- Are you meeting the industry benchmark for NPS Score?
- Have you identified areas for improvement based on patient feedback?
- Is your center leveraging advanced solutions to enhance patient experience?
By implementing targeted strategies and leveraging advanced solutions, such as those offered by Navikenz, your center can help you solve these problems, improve patient experiences and operational efficiency and achieve higher satisfaction & loyalty scores.
Contact us today to learn how we can help you transform your patient experience and achieve measurable improvements in satisfaction and loyalty at info@navikenz.com.
References
[1] https://urgentcareassociation.org/wp-content/uploads/2023-Urgent-Care-Industry-White-Paper.pdf
[2] https://customergauge.com/benchmarks/blog/nps-healthcare-net-promoter-score-benchmarks
[3] https://www.gmrwebteam.com/urgent-care-patient-satisfaction-survey-2021#:~:text=Overall%2C%20the%20Net%20Promoter%20Score,was%2077.30%20/100%20in%202020.
[4] https://www.jucm.com/nps-predicts-success-in-uc/
[5] https://customergauge.com/benchmarks/blog/nps-healthcare-net-promoter-score-benchmarks